Neuroscience
Epilepsy: Mapping the Link to Deep-Rooted Brain Circuits
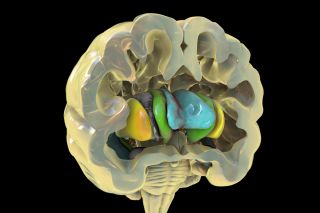
Lesion location mapping shows how epilepsy is linked to a subcortical network.
Posted July 10, 2023 Reviewed by Ray Parker
Key points
- Some people with brain lesions develop epilepsy; others don't.
- Lesion location mapping sheds light on how a brain lesion's location affects patients.
- Lesions that disrupt subcortical circuits linked to the cerebellum and basal ganglia increase epilepsy risk.
Neuroscientists have known for over a century that some (but not all) brain lesions cause epilepsy. Until recently, brain mapping had not revealed how the specific location of a brain lesion increases the likelihood of someone developing lesion-related epilepsy.
A new brain mapping analysis (Schaper et al., 2023) published in JAMA Neurology on July 3, suggests that lesional epilepsy is linked to a subcortical brain network with roots deep below the cerebral cortex's surface. Regardless of where a lesion is located, if it disrupts whole-brain functional connectivity with the deeply rooted cerebellum and basal ganglia, it's more likely to cause lesion-related epilepsy.
Conversely, if a brain lesion doesn't disrupt functional connectivity with this subcortical neural network, people's brains don't tend to experience epileptogenesis, and they're less likely to have spontaneous or chronic seizures. Epileptogenesis is a complex and not-fully-understood process that makes previously neurotypical brains prone to surges of abnormal electrical activity that cause epileptic seizures.
Deep-Rooted Subcortical Circuits Are Key to Epilepsy
Previous research (Gong et al., 2021) suggests that thalamocortical circuitry linked to the cerebellum and basal ganglia may act like a "brake" that controls epileptic seizures. Along these same lines, animal studies have found that optogenetic modulation and neurostimulation of the basal ganglia and cerebellum can reduce or terminate seizures in mouse models of epilepsy.
Human studies (Roa et al., 2022) suggest that targeting a mid-brain region called the thalamus—which acts like a relay station between cortical and subcortical areas underneath the cerebrum—with neurostimulation therapies, such as deep brain stimulation (DBS), or the NeuroPace Responsive Neurostimulation System (RNS), helps to control seizures.
Brain circuit mapping is key to locating and identifying the best targets for treating epilepsy via DBS and other forms of neurostimulation, such as transcranial magnetic stimulation therapy. (See Why Mapping Cerebellum-Prefrontal Cortex Circuitry Matters)
Lesion Location Mapping Can Pinpoint Neuromodulation Targets
In their latest retrospective analysis of brain mapping data, Schaper et al. focused on the research question: "Does lesion-related epilepsy map to a brain network?"
To answer this question, first author Frederic Schaper of Harvard Medical School's Center for Brain Circuit Therapeutics and an international team of colleagues, performed a brain mapping analysis called "lesion location mapping," using pre-existing data sets of 347 people with lesion-related epilepsy and 1,126 people who had brain lesions in different locations but didn't have epilepsy.

Their data analysis showed that lesion-related epilepsy maps to a brain network connected to the cerebellum and basal ganglia. The researchers found that those with lesion-related epilepsy were likelier to have lesions linked to this brain network. These findings suggest that disruptions of the cerebellum and basal ganglia's functional connectivity with other brain regions might be a root cause of lesion-related epilepsy.
Interestingly, deep brain stimulation that targeted areas connected to this brain network was associated with seizure control and "significant improvements" in 30 patients who underwent DBS for drug-resistant epilepsy.
"We're learning more and more about where in the brain epilepsy comes from and what brain circuits we need to modulate to treat patients with epilepsy," Schaper said in a release. "Using a wiring diagram of the human brain, lesion network mapping allows us to look beyond the individual lesion location and map its connected brain circuit."
Brain Maps Provide Clues About Lesion-Related Epilepsy; More Research Needed
During a neurological assessment, knowing that lesion-related epilepsy maps to a specific brain network linked to the cerebellum and basal ganglia could help doctors identify which patients with brain lesions are at higher risk of developing epilepsy based on a lesion's location. Soon, newly-charted brain maps might guide more precisely targeted neuromodulation to treat epilepsy effectively.
In their paper's conclusion, the authors note that "any clinical implications should be interpreted with caution, as our study was based solely on retrospective analyses of existing data sets." They also state that more research is needed "to determine if this [cerebellum/basal ganglia] network can be used as a clinical tool for prognosis or treatment of epilepsy."
References
Frederic L. W. V. J. Schaper, Janne Nordberg, Alexander L. Cohen, et al. "Mapping Lesion-Related Epilepsy to a Human Brain Network." JAMA Neurology (First published: July 03 ,2023) DOI: 10.1001/jamaneurol.2023.1988
Jinnan Gong, Sisi Jiang, Zhiliang Li, Haonan Pei, Qifu Li, Dezhong Yao, Cheng Luo. "Distinct Effects of the Basal Ganglia and Cerebellum on the Thalamocortical Pathway in Idiopathic Generalized Epilepsy." Human Brain Mapping (First published: April 08, 2021) DOI: 10.1002/hbm.25444
Jorge A. Roa, Marina Abramova, Madeline Fields, Maite La Vega-Talbott, Jiyeoun Yoo, Lara Marcuse, Steven Wolf, Patricia McGoldrick, Saadi Ghatan, and Fedor Panov. "Responsive Neurostimulation of the Thalamus for the Treatment of Refractory Epilepsy." Frontiers in Human Neuroscience (First published: July 15, 2022) DOI: 10.3389/fnhum.2022.926337




