Attention
When Must Kids With Neuropsych Symptoms See a Neurologist?
Caregivers should pay attention to root causes of neuropsychiatric symptoms.
Posted October 31, 2020 Reviewed by Ekua Hagan

Last week, I received a text message from a colleague: “Are you available for a short consultation? I have a case that does not add up.”
That’s an attention-getter for me. The comprehensive framework I’ve used for a decade—an all-wellness approach, I call it—emerged because some of my earliest cases were very complex. In trying to understand the failure of earlier interventions of many of my clients, I came face-to-face with the limitations of interventions that focus narrowly on one or only a few modalities of treatment.
When things “don’t add up," it means that a client is not responding as expected to an intervention. Often it’s because we’re looking too narrowly at a complex set of symptoms. I learned that it pays to expand my perspective in reviewing client symptoms and consider all aspects of wellness: emotional, cognitive, physical, spiritual, and social.
Onset of symptoms
My colleague's description: I spoke to a new client today, a child age 10 who displays the onset of significant debilitating symptoms. A few days ago he vomited and since then has refused to eat. He repetitively says: “I want to die," something he has never said before.
The parents are terrified and immediately contacted me for an intake. When I spoke with the boy, it was such an unfamiliar experience. Nothing that I said seemed to reach him; in fact, it only seemed to make things worse. Something doesn’t add up here. Could this be AE or PANDAS? (She had recently participated in my webinar on PANDAS).
My answer: Yes, it could be! I gave her the phone number of a neurologist who specializes in PANDAS/PANS/AE to follow up for immediate medical consultation.
Then my friend asked: How are you so quickly recognize that it could be PANDAS?
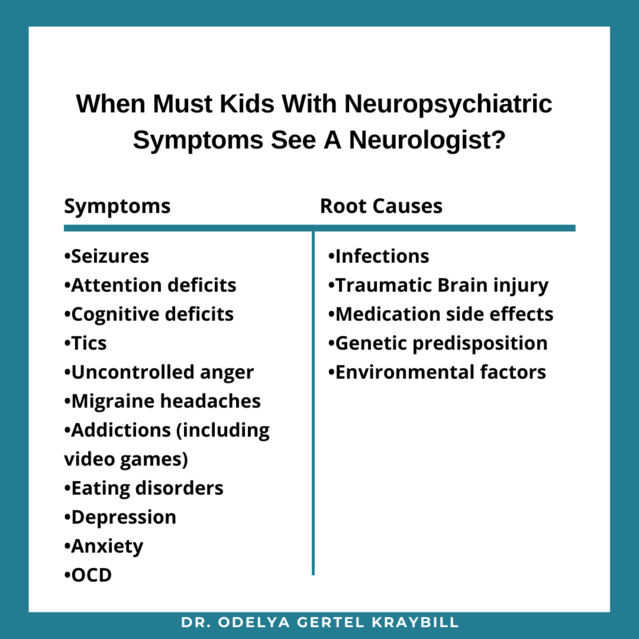
I reminded her of the things we had discussed in the webinar, in particular, the five possible root causes of neuropsychiatric symptoms that need to be ruled out before choosing interventions such as counseling or psychiatric intervention (see image below).
In this post, I’ll summarize things that parents and therapists should consider before assuming that therapy or psychiatric medications are the first lines of treatment for a child with neuropsychiatric symptoms.
Why It’s Important to Know When Neurological Evaluation Is Required
Neuropsychiatric root causes impact brain functions and manifests in dysregulation of mood, cognition, behavior, and movement. Potential symptoms include a wide range, from problems with focus and learning to sadness, aggressiveness, memory problems, sleep problems, depression, tics, seizures, and more. Here’s the danger: Since many of these symptoms look like common psychological symptoms, it’s easy even for highly trained professionals to misdiagnose the root causes of symptoms.
Children and teens with neuropsychiatric symptoms are often not well-suited to intervention modalities that rely solely on cognitive or behavioral methods as the first line of intervention. These methods engage the upper part of the brain; they assume that it can be sufficiently engaged to execute cognitive processing and behavioral changes. Unfortunately, this is not the case with most clients with neuropsychiatric symptoms.
For such children, we must instead begin with strategies for calming a child’s nervous system and building an interpersonal attunement with the child (parents-child, and or therapists-child). This work must be done in ways that enable the calming of the nervous system reactivity. Once that is accomplished, we can proceed to re-engage the upper brain and strengthen its functioning, and cognitive and behavioral methods have a useful role to play in this (more here).
When Is Neurological Evaluation Needed?
When children, teens, and young adults suffer from the following neuropsychiatric symptoms:
- Seizures
- Attention deficits
- Cognitive deficits
- Tics
- Uncontrolled anger
- Migraine headaches
- Addictions (including video games)
- Eating disorders
- Depression
- Anxiety
- OCD
Many of the families who end up in my clinic started with therapists who deploy only cognitive strategies, which didn’t work, for the reasons outlined above. Often the child is referred for psychiatric treatment. Drugs may reduce symptoms but they don’t bring resolution. This is tragic for some children, for it destinies them to spend their childhood years on powerful medications with significant side effects, while leaving underlying causes untouched.
Five Neurological Root Causes That Need to Be Ruled Out Before Choosing the Psychiatric Route
- Underlying infections. Rule out and treat underlying root causes that lead to neuropsychiatric symptoms and PANS/PANDAS and Autoimmune Encephalitis.
- Traumatic Brain Injury (TBI) can be an underlying root cause of a large number of neuropsychiatric problems.
- Medication side effects.
- Genetic predisposition.
- Environmental factors. Growing evidence demonstrates the impact of environmental exposure on brain development and as an increased risk factor for problems later. (Hollander et al., 2020).
A day after the conversation with my friend, she sent me a note: “You were right. The parents contacted a neurologist who sent them to the emergency room for immediate intervention for suspected autoimmune encephalitis."
I wish I had been wrong: Autoimmune encephalitis is a challenging condition for both the child and the entire family.
But it’s far better to know the real source and treat it than to chase around for years for answers. It is urgent that doctors, therapists, and parents be provided with accurate information about how to recognize and respond to neuropsychiatric symptoms in children, teens, young adults, and adults. The emotional and physical well-being of many thousands of people and their families depends on this.




